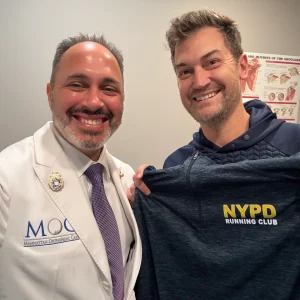
In the field of orthopedic research, Dr. Armin Tehrany continuously teams up with the best orthopedic experts to publish new findings. The primary goal of this collaborations is to provide extensive orthopedic studies, beneficial to all of his peers.
In May 2002, Dr. Tehrany partnered with Dr. Stephen S Burkhart and published Massive Rotator Cuff Tears: Results of Arthroscopic Partial Repair, an article featured in the online edition of Arthroscopy: The Journal of Arthroscopic & Related Surgery.
The Journal of Arthroscopic and Related Surgery is a leading peer-reviewed journal in the field of arthroscopic surgery. For orthopedic surgeons and orthopedic doctors, this journal is the most important source for extensive information in the field of arthroscopic surgery.
With every issue, the authors aim to provide detailed reviews on various emerging arthroscopic techniques. The articles feature detailed descriptions on the advantages and disadvantages of different arthroscopic methods. The online edition of the journal, along with the articles, feature video clips, short reports, and MEDLINE links to related articles as well.
The Massive Rotator Cuff Tears: Results of Arthroscopic Partial Repair article was published in 2002. It was featured in the May–June issue, 2002 Volume 18, Issue 5 edition, on pages 43–44. Following is a summary of the article.
Abstract
Introduction: We retrospectively reviewed a series of 12 patients in whom complete closure of a massive rotator cuff tear was not technically possible and an arthroscopic partial repair was performed.
Methods: There were 9 men and 3 women with an average age of 60.7 yrs. Indications for surgery included clinical and/or MRI-confirmed evidence of a rotator cuff tear. Average tear size was 5.4 x 6 cm. The operative technique was employed when complete repair was deemed impossible. After arthroscopic tendon mobilization, the torn posterior cuff tissue was shifted as superiorly as possible onto the greater tuberosity in order to achieve balanced force couples. Additional techniques, such as single or double interval slide were used when necessary. No tendon transfers or grafts were utilized.
Results: Average follow-up was 35.2 months (12-76 months). UCLA scores increased from 8.9 to 31.7 (p<.0001). Results were good or excellent 83% (10/12), fair 13% (2/12) and poor 0% (0/12). All patients described their pain as minimal to none. Average postoperative forward flexion was 160 degrees with all patients gaining overhead function. No patient lost active range of motion in this series. Three patients had reversal of proximal humeral migration. Of the two fair cases, one patient had a positive Napoleon sign indicating a subscapularis tear; the other patient was a revision case requiring a two-stage procedure. Overall satisfaction was 92%.
Conclusions: Arthroscopic rotator cuff repair, even when incomplete, provides pain relief and functional gains. The technique should be considered for tears that are otherwise deemed irreparable.